Welcome to the specialized, fast-paced world of endodontics! If you’ve just stepped into an endodontic office, you might feel like you’ve been dropped into a different language. While general dentistry covers everything from cleanings to crowns, endodontics is a “deep dive”—literally—into the internal health of the tooth.
Billing here isn’t just about clicking buttons; it’s about understanding the nuances of pain, pathology, and precision. If you’re feeling a bit underwater with all the D-codes and “irreversible pulpitis” talk, take a breath. This guide is designed to turn that overwhelm into expertise.
1. Mastering the Core Language: Endodontic Procedure Codes
In a general practice, you might juggle 200 different codes. In endo, you’ll live and breathe about 15. But because these procedures are high-value, a single coding error can cost the practice thousands.
The “Big Three” Root Canal Codes
-
D3310 (Anterior): Front teeth (1 root).
-
D3320 (Bicuspid): Middle teeth (1-2 roots).
-
D3330 (Molar): The complex ones (3+ roots).
Beyond the Standard Root Canal
You’ll also encounter surgical procedures like Apicoectomies (D3410–D3425). This is where the doctor accesses the root tip through the gum. These often require more detailed narratives because insurance companies love to ask, “Why didn’t you just do a standard root canal?”
CEO Insight: In my 13+ years of experience, I’ve seen offices lose revenue simply by miscoding D3331 (Incomplete endo). If a patient is non-restorable mid-procedure, you must know how to pivot the billing immediately so the chair time isn’t wasted.
2. The Golden Rule: Speed in Insurance Verification
Endodontics is an “emergency-driven” specialty. A patient calls at 9:00 AM in excruciating pain; they are in your chair by 10:30 AM.
The Challenge: You have 90 minutes to find out if they have met their deductible, if their “Missing Tooth Clause” applies (though less common in endo, it matters for replacements), and most importantly, if they have a waiting period.
Your Checklist for Every Call:
-
Frequency Limits: Most plans only cover one root canal per tooth per lifetime (or every 5-10 years). If you don’t check this, the claim will be denied as a “duplicate service.”
-
The “In-Progress” Rule: If a patient started a root canal with a general dentist and came to your specialist to finish it, who gets the “payday”? You must verify how the payer splits the fee.
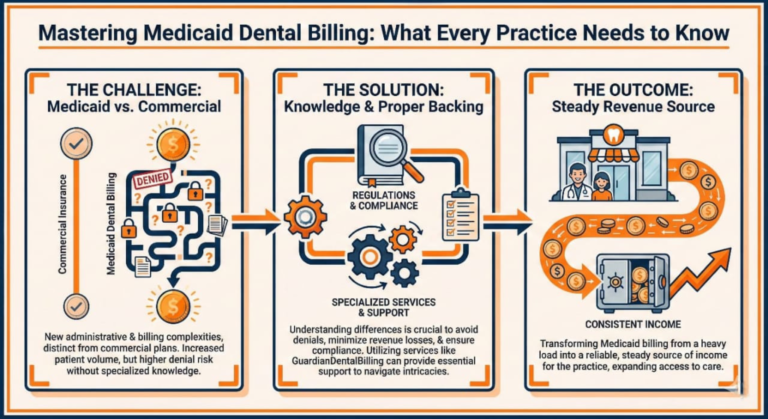
3. Medical vs. Dental: The “Gray Area”
Most of your work stays in the dental realm, but endodontists are oral surgeons of the pulp. When a patient comes in with a massive abscess that has spread to the jaw (cellulitis), you are suddenly looking at a medical situation.
When to think Medical (ICD-10):
-
Trauma: If a kid falls and knocks a tooth out (Avulsion), medical insurance often takes primary responsibility.
-
Diagnostic Imaging: Sometimes a CBCT (D0367) is medically necessary to find a hidden fracture that a 2D X-ray missed.
4. The Power of the Narrative
Insurance adjusters are looking for reasons to “downcode” your molar root canal to a bicuspid rate or deny it entirely. Your narrative is your defense attorney.
Don’t just write: “Tooth hurt, did root canal.” Do write: “Patient presented with lingering thermal sensitivity and spontaneous nocturnal pain. Radiograph shows periapical radiolucency on distal root. Prognosis: Good with endodontic intervention.”
5. Using Narratives and X-rays Strategically: The Art of the “Clean Claim”
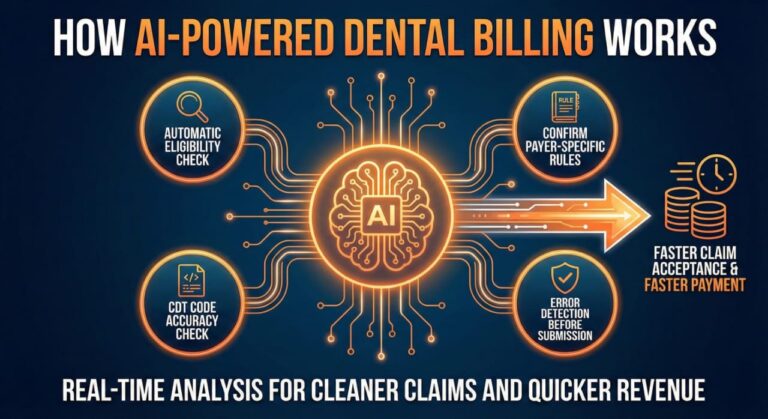
In endodontics, insurance companies don’t just take your word for it. They view every root canal as a high-cost event and will look for any reason to delay payment. This is where your 98% Clean Claim Rate begins.
The “Internal Audit” Mentality
Before you hit “submit” on a claim for a D3330 (Molar Root Canal), look at the X-ray through the eyes of an insurance adjuster. Is the decay visible? Is the radiolucency (the dark spot at the root tip) clear? If the X-ray is grainy or angled poorly, the claim will be pended for “additional information,” adding 30 days to your AR.
Writing Narratives that Get Paid
A narrative isn’t just a clinical note; it’s a justification for payment.
-
For Retreatments (D3346–D3348): You must explain why the original root canal failed. Use phrases like “previous endodontic therapy failing due to persistent apical periodontitis” or “calcified canals requiring microscopic intervention.”
-
For Cracked Teeth: If the doctor finds a fracture, document it with an intraoral photo if possible. Narratives should specify: “Fracture extends to the pulpal floor, necessitating endodontic therapy to retain the tooth.”
6. Track Tooth Numbers and “Phantom” Denials
It sounds simple, but tooth number errors are the #1 reason for “silent” denials—where the claim sits in a “rejected” status in your clearinghouse but never actually reaches the insurance payer.
-
The Supernumerary Trap: If an endodontist is working on an extra tooth (a supernumerary), you can’t just use numbers 1–32. You must use the correct supplemental numbering (51–82).
-
The “Same Day, Different Tooth” Issue: If a patient has two root canals on different teeth in the same day, many systems will flag the second one as a duplicate. You must use Modifier 77 or a clear narrative to distinguish that these are two separate surgical sites.
7. Coordinate with Referring Offices: Building the “Revenue Bridge”
As an endodontic biller, you are part of a larger ecosystem. The general dentist (GP) is your primary source of business. If your billing process is messy, it reflects poorly on the GP who referred the patient.
-
The “Insurance Info” Gap: Often, the referral slip has the wrong insurance or an old ID number. Don’t wait for the patient to arrive to fix this. Call the GP’s office and ask for a copy of the patient’s insurance card.
-
Closing the Loop: Once the root canal is done, the patient must go back to the GP for the final crown. Your billing notes should reflect that the “permanent restoration is to be completed by the referring provider.” This prevents insurance from thinking the root canal is “incomplete” because no crown was billed by your office.
8. Collect Payment Strategically: The “Financial First” Approach
Endodontics is expensive. A molar root canal and a core buildup can easily exceed $1,500. If you don’t collect at the time of service, your 90+ day AR will skyrocket.
The “Estimate” Conversation
Never say, “Insurance covers 80%.” Instead, say, “Your insurance typically contributes toward this procedure, leaving your estimated out-of-pocket portion at $350 today. How would you like to take care of that?”
Managing the “Patient Portion”
-
Real-time Processing: If your software (like Dentrix Ascend or Open Dental) allows for real-time claim adjudication, use it. Knowing the exact penny the patient owes before they leave the chair is the secret to Zero Pending Claims.
-
Financing Options: Since endo is often an unexpected emergency expense, always have CareCredit or Sunbit links ready.

9. Advanced Topic: Handling Denials and Appeals
Even with perfect coding, you will face denials. The difference between a struggling practice and a thriving one is the Follow-up Protocol.
-
The 14-Day Rule: Never let a claim sit longer than 14 days without a status check.
-
The “Peer-to-Peer” Appeal: If a claim for a complex apicoectomy is denied, don’t just resubmit the same info. Request a “Peer-to-Peer” review where your endodontist speaks directly to the insurance company’s dental consultant. This has a 90% success rate for complex cases.
10. Software Mastery: The Digital Backbone of Endodontics
Whether you are using Dentrix, Eaglesoft, Open Dental, or Curve Hero, the principles of efficient billing remain the same, but the “clicks” change. As a specialist’s office, you need to leverage these tools to automate the “grunt work.”
Dentrix (Ascend & Enterprise)
-
The Power of Templates: Create “Clinical Note Templates” for common endodontic diagnoses. This ensures that every root canal has the necessary narrative keywords (e.g., pulpitis, apical periodontitis) required for payment.
-
The Ledger Audit: In Dentrix, always use the “Check Audit Trail” if a claim is stuck. It often reveals if a tooth number was changed after the claim was created.
Open Dental
-
Custom Queries: Open Dental is the favorite of data-driven offices. You can write custom SQL queries to find “Procedures Not Attached to Insurance” with a single click. This prevents thousands of dollars from “slipping through the cracks.”
-
Unearned Splits: Master the “Split” feature. When a patient pays a large deposit for a root canal that spans two visits, ensure the payment is split correctly between the treatment and the final billing to keep your reports clean.
11. The “Advanced” RCM Metrics: How to Measure Success
To move from a beginner to a manager, you must stop looking at “Total Production” and start looking at Revenue Cycle Management (RCM) KPIs.
12. Conclusion: Your Role in the Practice’s Success
Endodontic billing requires a comprehensive understanding of the intricacies involved in coding and insurance reimbursements. This expertise not only streamlines the billing process but also ensures that patients receive the financial support they deserve throughout their treatment journey. Furthermore, proficient endodontic billing practices safeguard the financial interests of the practice by minimizing errors and optimizing revenue cycles. By demonstrating diligence in tracking outstanding claims and maintaining clear communication with insurance providers, billing professionals significantly enhance the overall efficiency of the front office. Ultimately, a well-executed endodontic billing strategy is essential for fostering patient trust and sustaining the financial health of the dental practice. .
Welcome to the specialty. It’s fast, it’s complex, but when the Zero Pending Claims report hits the doctor’s desk, it’s incredibly rewarding. Endodontic billing requires a comprehensive understanding of the intricate codes that govern insurance reimbursements. Each claim submitted is not merely a transaction; it represents a commitment to advocating for the patient’s financial well-being while safeguarding the practice’s revenue streams. Mastery of billing software and meticulous follow-up on claims ensures that every dollar is accounted for, reflecting the dedication and expertise of the front office. In this dynamic environment, your role transcends traditional billing; you become an essential ally in the financial health of both the patient and the practice.
What is the importance of precision in Endodontics Billing?
Precision in Endodontics Billing ensures that claims are processed accurately, minimizing the risk of denied claims and improving cash flow for the practice.
How can I keep my accounts receivable (AR) under 90 days in Endodontics?
Focus on the Big Three codes (D3310-D3330) and implement efficient insurance verification processes to maintain lower AR.
What is a Clean Claim in Endodontics Billing?
A Clean Claim is one that is submitted without errors and meets all payer requirements, achieving a gold standard acceptance rate of 98%.
Why is clinical narrative essential in Endodontics Billing?
Clinical narratives justify medical necessity, providing detailed explanations that support the need for specific procedures and enhancing the chances of claim approval.
How can software like Dentrix or Open Dental enhance Endodontics Billing?
These software solutions automate workflows, streamline billing processes, and improve accuracy in claim submissions, leading to greater efficiency in revenue cycle management.
What strategies can I use for emergency same-day billing in Endodontics?
Implement streamlined protocols for insurance verification and immediate claim submission to capitalize on emergency procedures, ensuring prompt reimbursement.
How do I handle complex procedures like apicoectomies in Endodontics Billing?
Document the clinical necessity thoroughly, use the appropriate billing codes, and provide supporting narratives to facilitate approval of complex claims.
What are the benefits of mastering the 10-minute insurance verification process?
Mastering this process allows practices to confirm patient eligibility quickly, reducing delays in treatment and improving overall patient satisfaction.
How does effective Endodontics Billing contribute to a thriving practice?
Efficient billing practices increase revenue, reduce claim denials, and enhance cash flow, ultimately supporting the financial health and growth of the practice.
What role does precision in the ledger play in maintaining an Endodontics practice?
Precision in the ledger ensures accurate financial reporting, reduces errors in billing, and helps maintain a steady cash flow, which is vital for the sustainability of the practice.